Comparison Between Cementless Bipolar Hemiarthroplasty and Proximal Femoral Nail Anti-Rotation for Unstable Intertrochanteric Femoral Fractures in the Elderly: A Retrospective Study
DOI:
https://doi.org/10.56929/jseaortho-2025-0193Keywords:
unstable intertrochanteric fracture of femur, cementless bipolar hemiarthroplasty, proximal femoral nail anti-rotation, mortality rate of hip fractureAbstract
Background: Proximal femoral nail anti-rotation (PFNA) is the gold-standard treatment for intertrochanteric fractures in elderly patients. However, some authors have recently recommended the use of cementless bipolar hemiarthroplasty (CLBHA) for unstable intertrochanteric fractures and achieved satisfactory results. This study aimed to compare the results and mortality rate postoperatively five years between CLBHA and PFNA for unstable intertrochanteric fractures of the femur in elderly patients (age > 60 years).
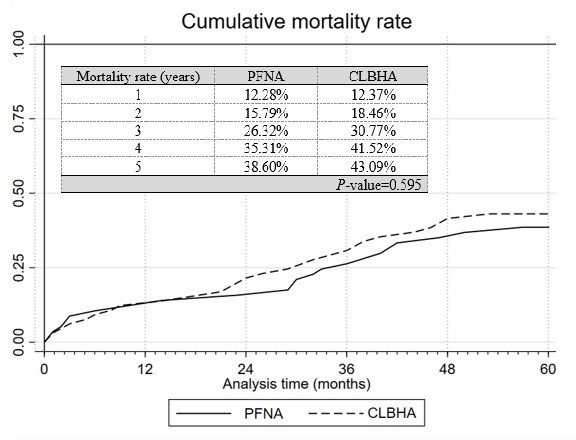
Methods: This retrospective study reviewed in and outpatient medical records and civil registrations between October 2012 and October 2017 at our hospital. In total, 122 patients (43 men, 79 women; aged 60–93 years) with unstable intertrochanteric femurs were treated. Fractures were divided into the CLBHA and PFNA groups. Differences in operative time, intraoperative bleeding, blood transfusion, ambulation-to-walk duration, postoperative hospitalization, postoperative complications and revision rate, ambulation at six months, and five-year mortality rate were collected. The unpaired t-test was analyzed using the χ2 test, and statistical significance was set at P < 0.05. The mortality rate is shown as an additional Kaplan–Meier estimate together with the p-value.
Results: The operative time (67.8±24.21 vs. 57±3.22 min, P =0.028), ambulation-to-walk duration with a gait aid (12.47±9.41 vs. 9.02±7.59 days, P <0.001), and postoperative hospitalization (911.55±6.61 vs. 7.11±3.45 days, P =0.037) were significantly different between the CLBHA and PFNA groups. Intraoperative bleeding, blood transfusion, postoperative complication, revision rate, ambulation at six months, and five-year mortality rate had no statistically significant differences.
Conclusions: Although CLBHA showed a longer surgical period, longer postoperative hospitalization, and slower ambulation compared to PFNA, the results showed no statistically significant difference in long-term outcomes and five-year mortality between both procedures for intertrochanteric femoral fractures in the elderly. Moreover, although PFNA remains the gold-standard treatment, CLBHA can be used as an alternative procedure in certain situations; however, the choice of procedure should depend on individual patient factors and surgeon expertise.
Metrics
References
Mithal A, Dhingra V, Lau E. The Asian Audit: Epidemiology, costs and burden of osteoporosis in Asia. Int Osteoporos Foundation 2009:24-9.
Suriyawongpaisal P, Pimjai S, Wichien L. A multicenter study on hip fractures in Thailand. J Med Assoc Thai 1994;77:488-95.
Chariyalertsak S, Suriyawongpaisal P, Thakkinstain A. Mortality after hip fracture in Thailand. Int Orthop 2001;25:294-7.
LeBlanc ES, Hillier TA, Pedula KL, et al. Hip fracture and increased short-term but not long-term mortality in healthy older women. Arch Intern Med 2011;171:1831-7.
Sahmir Sadic, Svemir Custovic, Mahir Jasarevuc, et al. Proximal femoral nail antirotation in treatment of intertrochanteric hip fractures. Med Arch 2015;69:352-6.
Hongku N, Woratanarat P, Nitiwarangkul L, et al. Fracture fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: A systematic review and network meta-analysis of randomized controlled trials. Orthop Traumatol Surg Res 2022;108:102838.
Kokoroghiannis C, Aktselis I, Deligeorgis A, et al. Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures--a review. Injury 2012;43:686-93.
McConnell JS, Saunders PRJ, Young SK. The clinical relevance of sound changes produced during cementless hip arthroplasty: a correctly sized femoral broach creates a distinctive pattern of audio frequencies directly related to bone geometry. Bone Joint J 2018;100-B:1559-64.
Homma Y, Zhuang X, Yanagisawa N, et al. Patients with shorter stature exhibit minimal hammering sound changes during cementless stem insertion in total hip arthroplasty. Arthroplast Today 2023;21:101136.
Jiamton C, Boernert K, Babst R, et al. The nail-shaft-axis of the of proximal femoral nail antirotation (PFNA) is an important prognostic factor in the operative treatment of intertrochanteric fractures. Arch Orthop Trauma Surg 2017;138:339-49.
Saini R, Jain M, Shah S, et al. Significant of tip apex distance (TAD) in proximal nail antirotation (PFNA) system used in trauma case of proximal femoral fractures. Int J Orthop Traumatol Surg Sci 2019;5:296-9.
Ruecker AH, Rueger JM. Pertrochanteric fractures: tips and tricks in nail osteosynthesis. Eur J Trauma Emerg Surg 2014;40:249-64.
Suriyawongpaisal P, Pimjai S, Wichien L. A multicenter study on hip fractures in Thailand. J Med Assoc Thai 1994;77:488-95.
Khunkitti N, Aswaboonyalert N, Songparanasilp T, et al. Fracture threshold in the Thai elderly and bone mineral density evaluation. J Bone Miner Metab 2000;18:96-100.
Han SK, Lee BY, Kim YS, et al. Usefulness of multi-detector CT in Boyd-griffin type 2 intertrochanteric fractures with clinical correlation. Skelet Radiol 2010;39:543-9.
Kim WY, Han CH, Park JI, et al. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 2001;25:360-2.
Huang X, Leung F, Xiang Z, et al. Proximal femoral nail versus dynamic hip screw fixation for trochanteric fractures: a meta-analysis of randomized controlled trials. Scientific World Journal 2013:2013:805805.
Setiobudi T, Ng YH, Lim CT, et al. Clinical outcome following treatment of stable and unstable intertrochanteric fractures with dynamic hip screw. Ann Acad Med Singap 2011;40:482-7.
Luo X, He S, Zeng D, et al. Proximal femoral nail antirotation versus hemiarthroplasty in the treatment of senile intertrochanteric fractures: Case report. Int J Surg Case Rep 2017;38:37-42.
Tan WL, Shi YX, Zhang, JY, et al. Bipolar Hemiarthroplasty should not be selected as the primary option for intertrochanteric fractures in elderly patients aged 85 years or more. Medicine (Baltimore) 2020;99:e21862.
Li J, Cheng L, Jing J. The Asia proximal femoral nail antirotation versus the standard proximal femoral antirotation nail for unstable intertrochanteric fractures in elderly Chinese patients. Orthop Traumatol Surg Res 2015;101:143-6.
Yang YH, Wang YR, Jiang SD, et al. Proximal femoral nail antirotation and third-generation gamma nail: which is a better device for the treatment of intertrochanteric fractures. Singapore Med J 2013;54:446-50.
Thakur A, Lal M. Cemented hemiarthroplasty in elderly osteoporotic unstable trochanteric fractures using fracture window. Malays Orthop J 2016;10:5-10.
Jayaram G, Sudhakar MV, Kumar RA, et al. Study of outcomes of cemented hemiarthroplasty for comminuted intertrochanteric fractures in the elderly. J Orthop 2023:41:67-72.
Donaldson AJ, Thomson HE, Harper NJ, et al. Bone cement implantation syndrome. Br J Anaesth 2009;102:18.
Duncan JA. Intra-operative collapse or death related to the use of acrylic cement in hip surgery. Anaesthesia 1989;44:149-53.
Govil P, Kakar PN, Arora D, et al. Bone cement implantation syndrome: A report of four cases. Indian J Anaesth 2009;53:214-8.
Haentjens P, Lamraski G. Endoprosthetic replacement of unstable, comminuted intertrochanteric fracture of the femur in the elderly, osteoporotic patient: a review. Disabil Rehabil 2005;27:1167-80.
Huang CG, Ye JJ. Comparison of three methods for the treatment of aged femoral intertrochanteric fracture. Zhongguo Gu Shang 2012;25:549-53.
Sniderman J, Vivekanantha P, Shah A, et al. Hemiarthroplasty for unstable intertrochanteric hip fractures: A matched cohort study. J Arthroplasty 2023;38:1522-7.
Chu X, Liu F, Huang J, et al. Good short-term outcome of arthroplasty with Wagner SL implants for unstable intertrochanteric osteoporotic fractures. J Arthroplast 2014;29:605-8.
Khamkhad A. Short metaphyseal femoral stem total hip arthroplasty in poor quality bone cortex without neck length sparing: A case report. JseaOrtho 2025;49:96-100.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.