Development of an Artificial Intelligence System for Hip Fracture Detection: A YOLOv8 Model Performance Study for Junior Orthopedic Surgeons
DOI:
https://doi.org/10.56929/jseaortho-2025-0263Keywords:
Hip fracture, YOLOv8, artificial intelligence, radiography, junior orthopedic surgeons, sensitivity, specificityAbstract
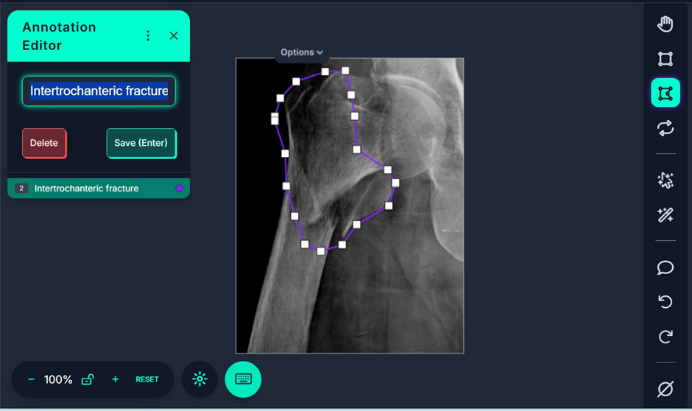
Purpose: Hip fractures represent a critical orthopedic emergency in the geriatric population; diagnostic delays or inaccuracies may result in severe morbidity and mortality. Contemporary artificial intelligence technologies demonstrate potential for precise and rapid radiographic interpretation, particularly in resource-constrained healthcare environments with limited availability of specialists. We aimed to develop and validate the diagnostic performance of a YOLOv8-based deep learning model by junior orthopedic surgeons for the detection of hip fractures, categorizing images into three classifications: normal anatomy, femoral neck fractures, and intertrochanteric fractures.
Methods: This retrospective study analyzed 2,035 anteroposterior hip radiographs from 942 patients. The YOLOv8 architecture was implemented using Google Colab with standardized hyperparameters. The dataset was stratified into training, validation, and testing sets. The performance evaluation utilized mean average precision (mAP@0.5), F1 score, precision, recall, sensitivity, specificity, and confusion matrix analysis.
Results: The YOLOv8 model achieved an mAP@0.5 of 0.879 and a maximum F1 score of 0.86. The model demonstrated a maximum precision, confidence threshold, and maximum recall of 1.00, 0.961, and 0.91, respectively, at a confidence threshold of 0.000. The sensitivity values were 97.7%, 87.0%, and 95.9% for intertrochanteric fractures, femoral neck fractures, and normal anatomy, respectively. The specificity ranged from 97.1% to 99.0% across all classifications, indicating exceptional screening accuracy, particularly for normal anatomy and intertrochanteric fractures.
Conclusions: The YOLOv8 model demonstrated clinical utility as a diagnostic screening tool for hip fractures, particularly in facilities with limited radiological expertise. However, femoral neck fracture classification requires further refinement through dataset augmentation and advanced training methodologies to enhance detection accuracy for this radiologically challenging entity.
Metrics
References
Sing CW, Lin TC, Bartholomew S, et al. Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J Bone Miner Res 2023;38:1064-75.
Shi BY, Hannan CV, Jang JM, et al. Association between delays in radiography and surgery with hip fracture outcomes in elderly patients. Orthopaedics 2020;43:e609-e15.
Pinto A, Berritto D, Russo A, et al. Traumatic fractures in adults: missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed 2018;89:111-23.
Lindsey R, Daluiski A, Chopra S, et al. Deep neural network improves fracture detection by clinicians. Proc Natl Acad Sci U S A 2018;115:11591-6.
Krogue JD, Cheng KV, Hwang KM, et al. Automatic hip fracture identification and functional subclassification with deep learning. Radiol Artif Intell 2020;2:e190023.
Cheng CT, Ho TY, Lee TY, et al. Application of a deep learning algorithm for detection and visualization of hip fractures on plain pelvic radiographs. Eur Radiol 2019;29:5469-77.
Beyaz S, Yayli SB, Kilic E, et al. The ensemble artificial intelligence (AI) method: Detection of hip fractures in AP pelvis plain radiographs by majority voting using a multi-center dataset. Digit Health 2023;9:20552076231216549.
Lee C, Jang J, Lee S, et al. Classification of femur fracture in pelvic X-ray images using meta-learned deep neural network. Sci Rep 2020;10:13694.
Beyaz S, Yayli SB, Kilic E, et al. Comparison of artificial intelligence algorithm for the diagnosis of hip fracture on plain radiography with decision-making physicians: a validation study. Acta Orthop Traumatol Turc 2024;58:4-9.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.